Remote monitoring must be part of the healthcare ecosystem
The GDP share of healthcare expenditure in many European countries has doubled over the last 50 years and is expected to continue to rise. Healthcare is one of the largest household expenses, whether it is financed jointly via taxes or as a separate fee to health insurance providers. In order to maintain broad acceptance for a jointly funded model and to manage the long-term financing of healthcare, we must bend the cost curve. Resources need to be used smarter and we must use technology better. We simply must do more for more people, without further increasing the pressure on healthcare staff or the cost base from which we do this.
In the Western world, about half of the population has a chronic disease, many live with two or more diseases. Care for people with chronic illness today accounts for a vast majority of healthcare costs. Tools and new ways of working are needed to meet the increased needs and to reduce pressure on the healthcare system. This is the key to preventing cost increases and managing long-term financing.
Today we talk a lot about digi-physical journeys, which are initiated with primary healthcare. When it comes to the more acute and mildly acute health conditions, development has been rapid, but the same requirements must apply to chronic care. The developmental trend towards close care is about increased accessibility, increased continuity, and improved opportunities to live a life with a high quality of life, even with chronic conditions. We are now seeing several different solutions, including those for remote monitoring, being tested and rapidly rolled out – but what should sustainable chronic care management based on digital technologies look like? I want to raise three points.
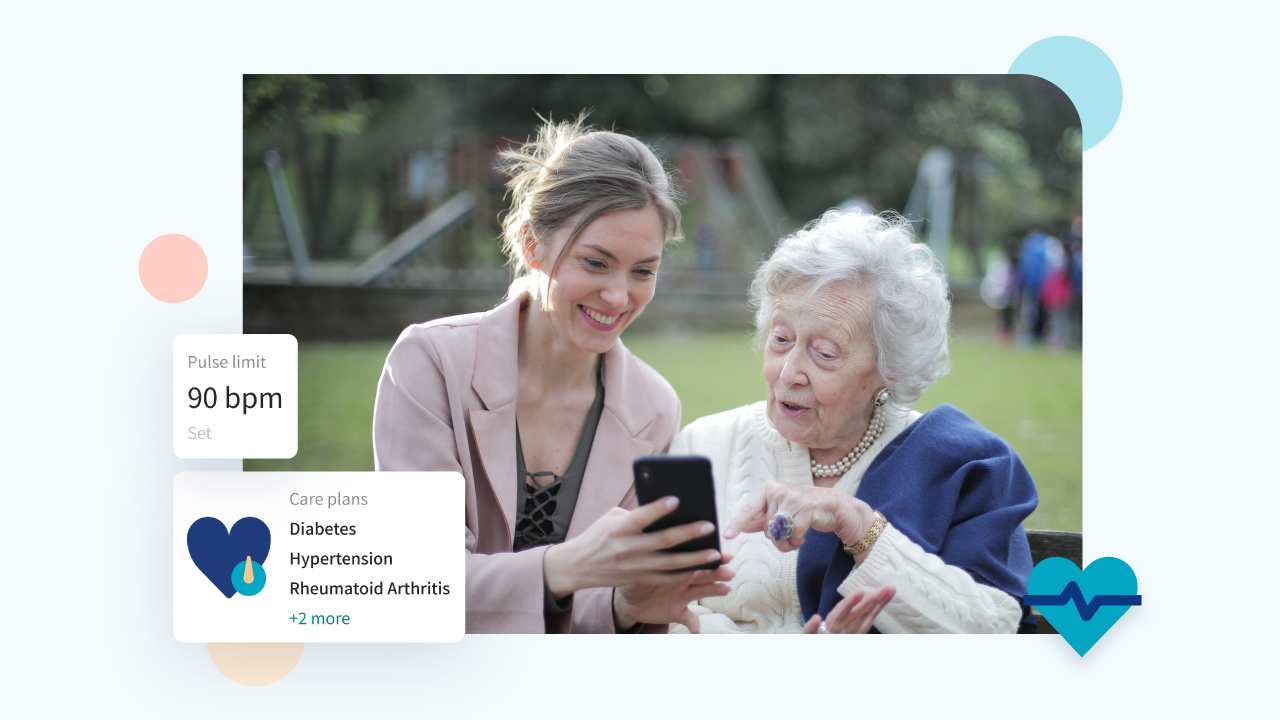
Solutions need to be Person-Centred and take as a starting point that a person is not a diagnosis, instead, they are an individual who can suffer from several different health conditions. One application for each condition resulting from a disease, which should then be linked to several different systems will not work. Not from a patient perspective, nor from a caregiver perspective.
Holistic patient journey. The focus must be on supporting whole journeys and creating a holistic patient experience even for chronic conditions. All components, including those that promote good health, need to be aggregated together so as not to create new verticals. Remote monitoring is just one of several components that must be included to create smart and sustainable digi-physical care and must be part of the larger healthcare ecosystem – not as an isolated function.
Scalability. The ambition must be to reach everyone who needs it with the technology available. Then it must be possible to scale up. Many small initiatives lead to non-standard, non-scalable applications, which makes it difficult to enable the fundamental journey we all need to make.
Digitalisation is an infrastructure issue and can be compared with how to build the ”railway” for a system. A foundation that is then further developed, must support all types of care journeys. Remote monitoring, which is part of a much larger digi-physical flow, must be built into the ecosystem solutions that are about to be put into place.
This is the way forward for creating smart digi-physical care, the key to bending the cost curve and managing long-term healthcare financing.