Pathways
Achieve better outcomes and increase cost-efficiency with care planes for elective and chronic care.
Create care plans in minutes
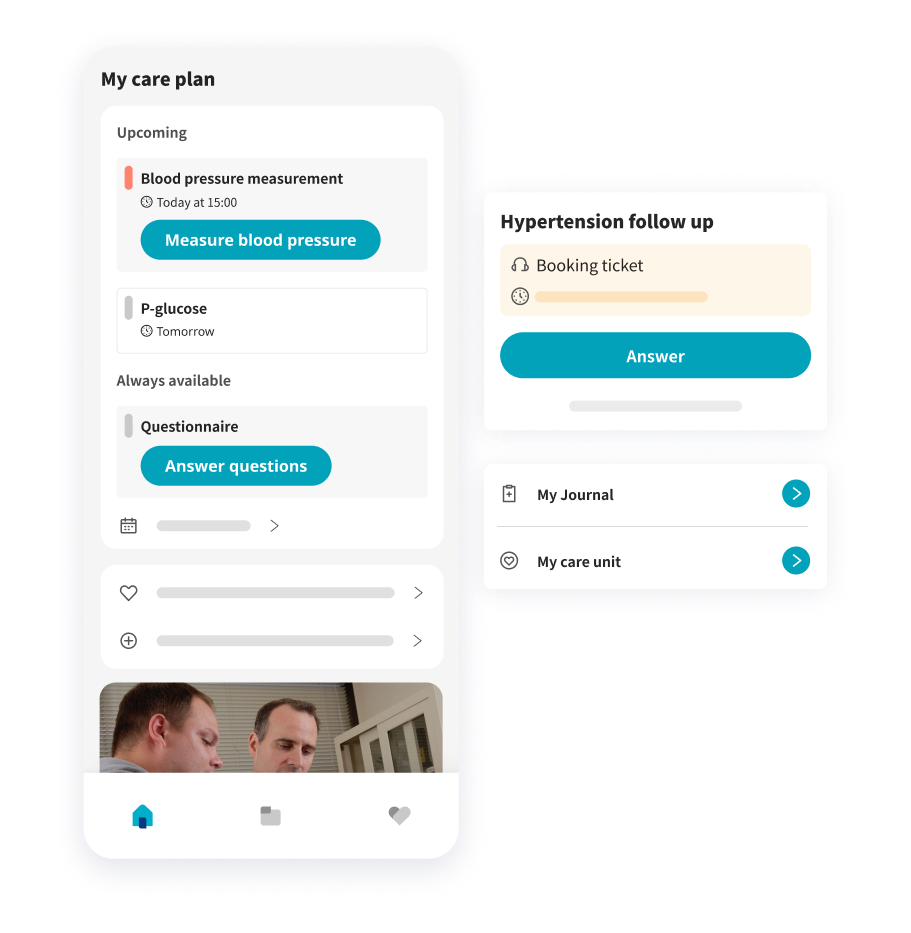
Platform24 Pathways is an efficient and easy to use way of creating careplans, for individuals or groups of patients. The solution offers full flexibility, allowing you to use standard care plans off the shelf, or build your own by combining medical questionnaires and hardware data.
Care plans for chronic and elective treatment
The Platform24 Pathways solution has two main use cases:
Recurring care plans for chronic care
By gathering and visualizing health data Remote Patient Monitoring (RPM) empowers patients to actively engage in their care, and provides practitioners a holistic view for proactive care prioritization.
- Hypertension
- Heart failure
- COPD
- IBD
- Etc.
Sequential care plans for elective care
Pathways drives efficiency by automating patient interactions, data collection, and administrative tasks pre and post surgery or treatment. This enables close collaboration among primary care, specialist care, and patients.
- Pre and post surgery
- Pregnancy
- Rehabilitation
- Cancer
- Etc.
Pathways and RPM flows
Full flexibility solution
Use standard care plans off the shelf, or build your own by combining medical questionnaires and hardware data.
Track and share vital signs
Allow patients to track their vital signs and symptoms, and to share this information with their healthcare team – in real-time. Working preventively not only helps patients receive care before issues develop more seriously, it also reduces potentially costly interventions.
Keep patients out of the hospital
With Pathways, healthcare providers are able to keep patients under supervision without frequent in-person visits. This is particularly important for patients with conditions requiring monitoring on a daily or hourly basis. It also saves patients plenty of time not having to travel.
Pathways as part
of the full care flow
We believe in remote monitoring as part of the overall healthcare journey in order to offer the best possible level of patient service and medical safety.
With Platform24, your patients can interact with you from one entry point – regardless of the reason for reaching out. Self-monitoring is managed in the same app they would use to seek other care, access lab results, read their journal, and much more.
Main benefits with Pathways
Patient experience, availability and flexibility
For chronic patients with RPM tools, assistance from their care provider is just one click away with an open asynchronous messaging channel. The first staff member to respond can see the patient’s full health status and quickly decide how to prioritize their case.
Medical safety
Many chronic patients only have one or two physical interaction points per year with healthcare workers, although they live with their conditions 365 days a year. With Pathways, the patient is offered the security of constant care presence, while the clinician also gets drastically increased amounts of data points.
Cost savings
With the opportunity to handle more patients through automated workflows, decision support, medical note suggestions, batch assessments, etc., the clinician can spend more time on patients and less time on administration, saving costs and making everyday life easier.
Staff satisfaction
Automated administration and batch assessment of routine cases offer practitioners more time to cultivate the patient/practitioner relationship and more time to dive deeper into challenging medical cases.
Pathways product series
Allows patients to report their subjective symptoms or the results from medical devices through questionnaires. The wide range of questionnaires and flexibility of the platform enables care processes which are adapted to the patient as well as the clinician.
This means pathways that are actually used by patients, that save time for clinicians and that improve quality of care.
Manual data reporting
Standardised forms for all data not automatically updated from HW
- Qualitative and subjective data (e.g. depression forms)
- Objective data from unsupported hardware
PROM
Standardised forms for PROM (Patient Reported Outcome Measures)
Clinician interface for
Care plan builder
Define care plans and care groups
Care plan manager
Manage groups of patients with chronic conditions
Medical data analysis
Follow individual patients over time through consumable data representations
Individual threshold limits
No one-size-fits-all: possibility to set individual thresholds based on age, gender or other factors
Auto-attestations
Value considered normal are automatically attested, allowing clinicians to only spend time looking at critical values that needs attention
Trend analysis
MDR certified algorithm analysing trends, making it possible to only flag the values considered as outliers for the patient
Adaptive logic
Questionnaires that are automatically sent out can be adapted based on the values reported by the patient. Also the frequency of future measurements can be adapted this way.
Automatic customised messages
Automatically send customised messages to patients depending on what values they report
The hardware integrations supported by Platform24 can be used as input for many different pathways, such as
- Hypertension
- Heart failure
- Asthma
- IBD
- Diabetes type II
- Etc.
All hardware devices supported by Platfom24 allow for automatic, wireless data transfer to the app.